Normal Delivery
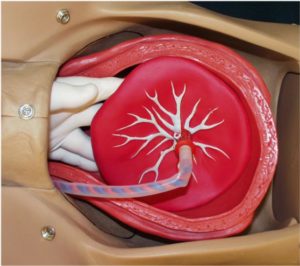
Immediately after delivery of the baby, the placenta is still attached inside the uterus. Some time after delivery, the placenta will detach from the uterus and then be expelled. This process is called the “3rd stage of labor” and may take just a few minutes or as long as an hour.
Signs that the placenta is beginning to separate include:
- A sudden gush of blood
- Lengthening of the visible portion of the umbilical cord.
- The uterus, which is usually soft and flat immediately after delivery, becomes round and firm.
- The uterus, the top of which is usually about half-way between the pubic bone and the umbilicus, seems to enlarge and approach the umbilicus.
Immediately after the delivery of the baby, uterine contractions stop and labor pains go away. As the placenta separates, the woman will again feel painful uterine cramps. As the placenta descends through the birth canal, she will again feel the urge to bear down and will push out the placenta.

If the placenta is not promptly expelled, or if the patient hemorrhages while awaiting delivery of the placenta, this is called a “retained placenta” and it should be manually removed.
After delivery of the placenta, the uterus normally contracts firmly, closing off the open blood vessels which previously supplied the placenta. Without this contraction, rapid blood loss would likely prove very problematic or worse.
To encourage the uterus to firmly contract, oxytocin 10 mIU IM can be given after delivery. Alternatively, oxytocin 10 or 20 units in a liter of IV fluids can be run briskly (150 cc/hour) into a vein. Breast feeding the baby or providing nipple stimulation (rolling the nipple between thumb and forefinger) will cause the mother’s pituitary gland to release oxytocin internally, causing similar, but usually milder effects.
A simple way to encourage firm uterine contraction is with uterine massage. The fundus of the uterus (top portion) is vigorously massaged to keep it the consistency of a tightened thigh muscle. If it is flabby, the patient will likely continue to bleed.
Retained Placenta
After delivery of the baby, the placenta normally detaches from the inside of the uterus and is expelled, often with additional pushing efforts by the mother. Normally this occurs within a few minutes of delivery of the baby, but may take as long as an hour.
The four signs of placental separation are:
- Apparent lengthening of the visible portion of the umbilical cord.
- Increased bleeding from the vagina.
- Change in shape of the uterus from flat (discoid) to round (globular).
- The placenta being expelled from the vagina.
Commonly, after about 30 minutes of waiting or if there is increased bleeding without evidence of placental separation, a manual removal of the placenta is undertaken. Anesthesia (regional or general) is typically used for this as manual removal can cause considerable abdominal cramping. Sometimes, IV narcotic analgesia will prove helpful in relieving this discomfort
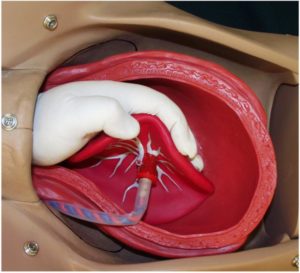
Manual Removal of the Placenta
One hand is inserted through the vagina and into the uterine cavity.
- Insert the side of your hand in between the placenta and the uterus. You may need to push through the placental membranes to accomplish this.
- Using the side of your hand, sweep the placenta off the uterus.
- After most of the placenta has been swept off the uterus, curl your fingers around the bulk of the placenta and exert gentle downward and outward traction. You may need to release the placenta and then re-grab it.
- Then pull the placenta through the cervix. Most placentas can be easily and uneventfully removed in this way. A few prove to be problems.
Placenta Accreta and Percreta
When you manually remove the placenta, be prepared to deal with an abnormally adherent placenta (placenta accreta or placenta percreta). These abnormal attachments may be partial or complete.
If partial and focal, the attachments can be manually broken and the placenta removed. It may be necessary to curette the placental bed to reduce bleeding. Recovery is usually satisfactory, although more than the usual amount of post partum bleeding will be noted.
If extensive or complete, you probably won’t be able to remove the placenta in other than handfuls of fragments. Bleeding from this problem will be considerable, and the patient will likely end up with multiple blood transfusions while you prepare her for a life-saving, post partum uterine artery ligation or hysterectomy. If surgery is not immediately available, consider tight uterine and/or vaginal packing to slow the bleeding until surgery is available.